One of the most severe effects of prolonged harmful alcohol use is alcohol-related liver disease. It progresses gradually, and it is not always detected. By the time alcohol-related liver disease is diagnosed, signs of liver failure may already be present. Understanding the onset, progression, and impact of liver disease on the human body can significantly help individuals seek assistance immediately and prevent long-term effects.
In this blog, we are going to discuss the causes, symptoms, tests, treatments, complications, prevention and support of alcohol-related liver disease. Consulting a liver specialist – Leaders in Liver Health- will help you identify and interpret the warning signs.
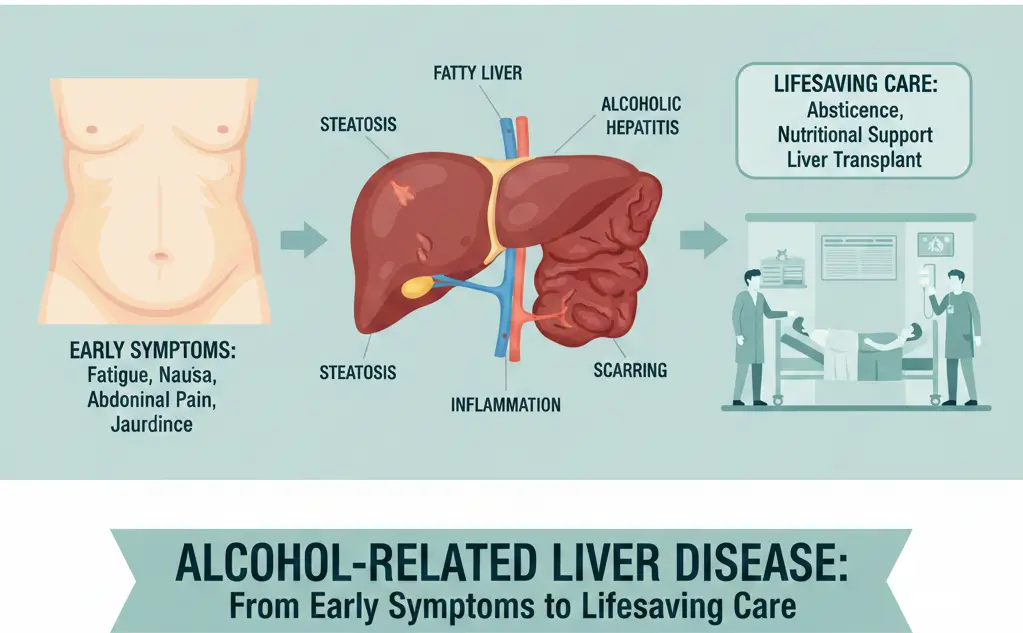
Alcohol exerts a significant strain on the liver. Whenever you consume alcohol, the liver works to break down the toxins. With time, alcohol excess causes fat deposition, inflammation, and scarring. This damages liver cells, rendering the organ unable to perform its functions properly. Persistent inflammation and scarring gradually reduce liver function, leading to conditions such as “fatty liver”, cirrhosis and alcoholic hepatitis. Various signs and symptoms are often present before people realise they have significant liver damage.
Not everyone who consumes alcohol to excess will develop alcohol-related liver disease. Genetics, gender, diet, and overall or general health also affect the liver. Liver damage among women can develop at lower levels of alcohol consumption when compared with men. Some individuals are more sensitive to the toxic effects of alcohol, this observation combined with poor nutrition, smoking, and obesity can accelerate or exacerbate liver damage. Long-term and harmful alcohol consumption can result in symptoms of liver disease appearing earlier and often quickly.

The alcohol-related liver disease occurs in stages:
Every stage increases the probability of the complications of chronic liver disease.
Heavy drinkers are prone to malnutrition, and this aggravates and accelerates liver damage. An unhealthy diet also undermines the immune system and impairs the liver’s ability to repair itself. Liver damage is also worsened by conditions such as diabetes, high cholesterol, or chronic infections. These are common factors that can exacerbate and complicate chronic liver disease due to harmful alcohol use.
The following are the symptoms of liver disease:
Early symptoms of alcohol-related liver disease are often vague or mild. As a result, many people do not notice these symptoms. The most common symptoms of liver disease are fatigue, loss of appetite, nausea, stomach ache, and weight loss. These are the initial symptoms that physicians can detect.
The symptoms are more evident when the liver is inflamed. Individuals can present with jaundice, abdominal distension, fever, vomiting, and loss of energy. This phase can be life-threatening. Other alarm symptoms observed in severe inflammation or alcoholic hepatitis include vomiting blood (haematemesis), or bleeding of the gastrointestinal tract.
In cirrhosis, scar tissue replaces healthy liver cells. Some of the symptoms are fluid retention (abdominal distension), easy bruising, confusion, itching, and muscle loss. Problems with thinking, concentration and memory often develop. At this stage, weak blood vessels and clotting problems with bleeding, vomiting blood, rectal bleeding or blood in the urine.
When bleeding occurs, confusion may intensify, or jaundice may develop rapidly, which often reflect life threatening symptoms. Episodes of acute vomiting (or vomiting blood), disorientation or swelling of the abdomen should be treated urgently.
Liver disease can be diagnosed through the following exams and tests:
Blood tests are used to determine levels of liver enzymes, clotting factors, indicators of inflammation, and blood protein levels. These tests assess liver function. The symptoms associated with harmful alcohol use often confirm the abnormal results indicative of liver disease.
Imaging assists in detecting scar tissue, enlarged veins, fatty changes, and liver structural abnormalities. The first test is usually an abdominal ultrasound scan, with a CT or MRI scan used to provide more information about the extent of liver disease.
A liver biopsy provides a small amount of liver tissue to examine under the microscope to identify the level of scarring or inflammation. Additional tests may include an endoscopy to exclude the presence of varices (or enlarged bleeding veins).
Physicians will inquire about the level of alcohol consumption, conduct screening tests, and examine the biological indicators. Assessing the level of alcohol consumption is crucial to establish a diagnosis and plan effective treatment.
Consult a Specialist
Dealing with symptoms or already diagnosed? Get expert care.
Consult a Alcohol-related Liver Disease Specialist Today
Personalized evaluation, evidence-based treatment plan, ongoing support.
For initiating the treatment, the following steps are helpful.
Stopping drinking is the most significant intervention. This will allow the liver to heal and prevent further damage. For alcohol-related liver disease, abstinence from alcohol is the most important step towards recovery.
Excessive alcohol consumption causes loss of vital vitamins in the body. It can be treated with vitamin supplements (particularly the B vitamins), high-protein foods, and the input of a specialist Dietician.
Doctors can prescribe specific drugs to aid the liver and this often requires the treatment of infection or the complications of chronic liver disease such as ascites, confusion or bleeding.
When the damage becomes permanent, a liver transplant may be the only treatment option. Liver transplantation is a last resort, which is reserved for those people who have stopped alcohol consumption and have met the rigid medical and psychological standards for organ transplantation.
Counselling and Support for Alcohol Withdrawal
Alcohol withdrawal can be dangerous in its own right. Patients can be assisted to abstain from alcohol through appropriate medical supervision, counselling and medication.
Recovery programs assist individuals to remain sober or teetotal. These groups provide emotional support, structure and guidance.
Liver health groups provide information, resources, and support for individuals with any liver disease.
Loved ones contribute significantly towards recovery. Family members can play a key role with appointments, lifestyle changes, and emotional well-being.
Online Forums for Long-Term Motivation
Online sobriety, liver health and long-term recovery groups are sources of motivation and provide a “connection” with other people.
Alcohol-related liver disease can be treated if it is detected early. The liver is capable of healing when alcohol consumption is stopped.
With cessation of drinking, many of the symptoms can disappear. Long-term liver health is supported by healthy living, frequent check-ups, and a proper diet.
In some cases where cirrhosis develops, there is limited reversal of the liver damage. Treatment of liver disease is often aimed at reducing disease progression and averting or managing it’s complications.
Follow-up appointments allow you to manage symptoms, monitor progress, and minimise the risk of relapse.
Liver failure can lead to the accumulation of fluid in the abdomen. This is something that needs to be managed urgently.
Life threatening bleeding or vomiting blood (haematemesis) results from high pressure in the blood vessels of the liver, known as portal hypertension.
As the liver is unable to remove toxins, they accumulate in the bloodstream, and interfere with brain function. This can result in confusion, drowsiness and personality change.
Long-term liver damage increases the risk of liver cancer. The presence of cirrhosis mandates surveillance for liver cancer.
Seek medical attention immediately for jaundice , uncontrolled abdominal swelling or pain, vomiting, or confusion related to liver disease.
Alcohol withdrawal may result in seizures, confusion, and heart problems. Medical attention is necessary.
In case of rapidly progressive symptoms, seek medical assistance or call an ambulance.
In case of rapidly progressive symptoms, seek medical assistance or call an ambulance.
Reduction of alcohol consumption is critical to avoid alcohol-related liver damage. Limiting the alcohol load on the liver can minimise long-term risks. Quitting drinking is necessary for people who are already experiencing the signs or symptoms of liver disease. The NHS suggests safe drinking guidelines of not more than 14 units per week.
Good nutrition helps restore liver health and its function. A healthy diet containing sufficient protein, vitamins, and fluids can facilitate recovery.
Regular examinations enable the physician to identify liver complications early, even when symptoms are mild or even absent. Frequent observations contribute to tracking changes over time and to timely intervention. Early testing helps avoid the severe complications of chronic liver disease.
Viral hepatitis can aggravate damage and accelerate liver disease. Vaccinations are available via the NHS that help prevent viral hepatitis (type A & B). Early diagnosis of viral hepatitis is achieved through screening.
Exercising regularly reduces strain on the liver and enhances overall well-being. Smoking prevention, engaging in physical exercise, and maintaining a constant healthy weight are measures that help protect the liver. Minor and regular adjustments can have long-term advantages.
Yes. Alcohol may cause irritation of the stomach and bowel lining, aggravate haemorrhoids and gastritis. Excessive or prolonged alcohol use may also impair liver function. Alcohol-related liver damage can result in impaired blood coagulation and increases the risk of bleeding. Rectal blood loss needs to be investigated without delay
Liver damage secondary to alcohol may start sooner than most individuals suspect. Frequent alcohol consumption that exceeds the UK recommended limit of no more than 14 units per week, increases the risk of liver disease. Consuming large quantities of alcohol over short periods, engaging in frequent binge drinking, or daily consumption can lead to “fatty liver”, fibrosis, cirrhosis and alcoholic hepatitis. Some individuals may be more susceptible due to genetics, weight, or other health conditions.
Yes. With abstinence from alcohol, good nutrition, and appropriate medical intervention for fatty liver and inflammation, can improve liver health. More severe scarring (cirrhosis) can be irreversible, highlighting the need for early detection and intervention. However, with alcohol cessation, the complications of chronic liver disease can be averted. The most significant difference is made through early diagnosis.
Consult a hepatologist urgently in case of jaundice, abdominal swelling, vomiting blood, black stools, extreme fatigue, unexplainable weight loss, or abnormal liver blood tests.
At present, the UK transplant centres demand total abstinence from alcohol, medical stability and a sense of dedication to long-term recovery. Assessments for liver transplantation are undertaken at dedicated transplant centres (or their spokes) and involve psychological and addiction support assessment. Leaders in Liver Health will investigate your liver disease and agree a personalised management plan to meet your individual needs.
Subtle Symptoms Need Expert Eyes
Many liver problems start with vague symptoms that are easy to dismiss. Our specialists are trained to recognise early warning signs and can investigate properly when something doesn’t feel right.
Don’t ignore your body’s signals – get expert assessment.
WhatsApp us